HIV infection is one of the most dreaded diseases that emerged in the late 20th century. Since the early days of its detection, it has wreaked havoc on mankind and has claimed many famous people as its victim. However, in the 21stcentury, many new medicines have been found useful in treating HIV, which has decreased the morbidity and mortality associated with HIV infections, tremendously.
It is estimated that approximately 21 million people around the world take life-saving antiretroviral therapy regularly. These medicines are very useful for reducing the amount of viral load in the blood of patients to very low levels and their chances of passing the virus to others are also lowered significantly. Antiretroviral therapy also prevents HIV from progressing to AIDS. But are these medicines always absolutely safe? Can there be a disease-free state, without taking any medicines? This article is just an attempt to answer, these life-changing questions, which are indeed a question of life and death for many unfortunate people.
Unfortunately, HIV treatment and side effects of antiretroviral drugsbecomea thing of secondary importance, when compared to the signs & symptoms of the HIV & fear of AIDS. The medications used in these conditions can cause serious side effects, which are mostly overlooked, in the grand scheme of things. In the past, these side effects were a major reason causing discontinuation of therapy or nonadherence to the strict schedule. With the newer antiretroviral therapy, incidences of serious side effects have relatively decreased, but have not disappeared entirely.
The major side effects of some common drugs used for the condition are – appetite loss (drugs like - zidovudine and abacavir), Lipodystrophy – characterised by loss or gain of fat in certain body areas (caused by drugs like – zidovudine, stavudine, didanosine and lamivudine), Fatigue (Zidovudine & efavirenz), Increase in Cholesterol level (zidovudine, stavudine, didanosine, saquinavir), Depression and mood changes (rilpivirine & efavirenz), Difficulty in sleeping (indinavir, efavirenz, rilpivirine), Nausea and vomiting (almost all drugs for treating HIV) and Diarrhoea.

According to a rough estimate, there are around 36 million people worldwide who are infected with HIV. Although a vast majority of them are stable and healthy with medications, chances of complications of drugs are always present. Besides, to keep millions of people dependent on medications for their entirelife also puts a lot of pressure on the drug delivery system and has very high maintenance costs involved. Due to these complications, a search for finding a permanent cure has always interested scientists, in which a need for taking medications for the rest of the patient’s life is no longer mandatory.
Although hard to believe, but finding a cure for HIV infection may be one of the greatest milestones in the history of medicine. In a miraculous turn of events, this has come true for an individual. “HIV cured by bone marrow transplant” – was news, reported by multiple media outlets in March 2019. Since the time of the beginning of this global epidemic, it is only for the second time, that it has been possible for aperson to be cured of HIV. So, what is this new treatment and how does this work? To understand the answer, we have to take a couple of steps back in time.
The patient, who has not been named and is described in the scientific community as “London patient”, suffered from HIV infection and had developedlife-threatening cancer (Hodgkin’s lymphoma), for which bone marrow transplant was given. The doctors responsible for the procedure attempted to clear the HIV infection, bytracing back the steps of a one of its kind of procedure, which was tried successfully 12 years back in another patient (The Belin patient). The method used was - Bone marrow transplant to treat HIV. The donor from whom the transplant was undertaken, had a rare genetic mutation of the CCR5 gene, which made a person HIV resistant.
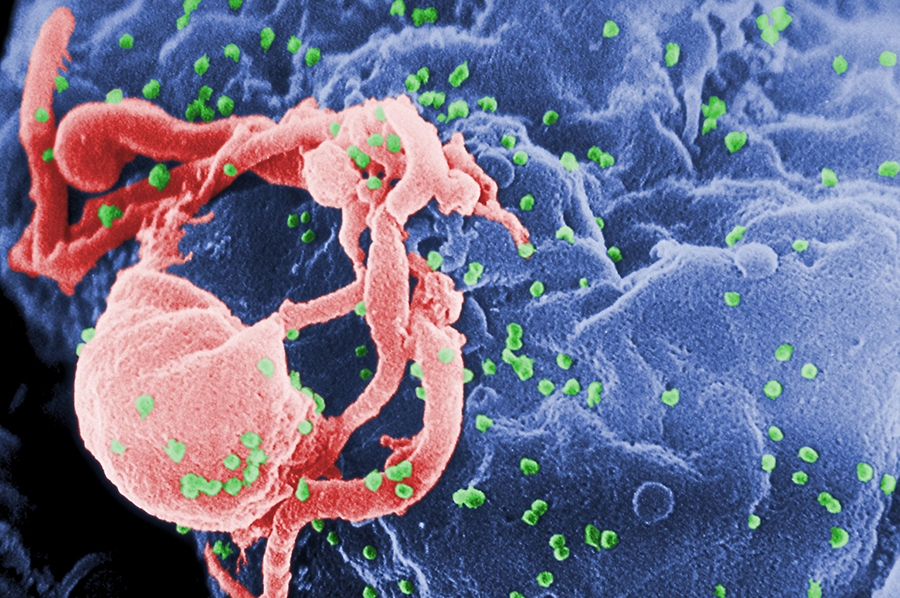
To understand CCR5 better, a short note on how it works would be helpful. Research has shown that HIV uses CCR5, which is a protein present on the surface of white blood cells (which forms a very important part of human immune system), to enter the cell and infect it. However, lot many people in the world (including almost 10% of the population of Europe), have a mutation, that changes the superficial location and size of the protein. So, when a mutation of CCR5 is present, HIV can’t latch on to these cells and infection of the human immune system is prevented.
Scientists believe that when the bone marrow transplant from the donor was undertaken, the donor immune cells also attacked the recipient’s immune cells, which may have been responsible for the loss of HIV infected cells. The London patient, continued the antiretroviral therapy for 16 months after the bone marrow transplant, before a decision was taken, to stop the drugs. Fortunately, his treatment course was relatively, much smoother, compared to the – Berlin patient, who had undergone the same treatment 12 years back, before emerging as the first example of “Cure for HIV infection”.
The medications were discontinued under medical supervision for 18 months, without any signs or symptoms of return of HIV. This has made many scientists believe methods of applying CCR5 gene editing in HIV patients, was a promising option, in pursuit of the search for the final cure.
1) Berlin Patient– The first successful incidence of Bone marrow transplant to treat HIV, was reported during a conference in the year 2007. The name of theperson to be cured of HIV was not disclosed & just described as “Berlin patient” by the scientific community (Although later the gentleman came forward to encourage other people afflicted by the same condition, & has been identified as 52-year-old Timothy Ray Brown).
He was suffering from leukemia, and bone marrow transplant (involving stem cells, which give rise to other blood cells) was done, when chemotherapy failed to give satisfactory results, forcancer treatment. The recovery phase was not smooth and he suffered from serious complications (including an induced coma), as side effects of strong immunosuppressive medications. Luckily, in spite of this near-death experience, he was finally cured and was free to lead a productive life without anti-retroviral medications.
The success of this incident prompted many other scientists to duplicate, this “HIV cured by bone marrow transplant” story, with little success. However, in all cases after stoppage of antiretroviral therapy, the virus came back; in some other cases, the patient succumbed to cancer. This lead many researchers, to believe that the Berlin patient, was a miracle, something that can never happen again. However, the success story of the London patient has changed this misconception.
2) Chinese Gene Edited Baby – World’s first gene edited babies (twin babies) were born on 26 November 2018, by efforts of a gene-editing researcher, working at the Southern University of Science and Technology of China, Shenzhen. The aim of this experiment was to make the babies, resistant to HIV infection.

To achieve the above-mentioned goal, the Chinese scientist, He JianKui, undertook an experimental procedure of gene edition, to disablethe CCR5 gene, which disabled the genetic pathway HIV uses to infect cells. Then this modified embryo was used to impregnate a woman. The babies born were resistant to HIV. However, because of subjecting the babies to unnecessary risks, and breaking the moral code of conduct of the scientific community, he was criticized around the world.
Although some health professionals were celebrating this great leap ahead, many experts have advised proceeding with caution. The scientific community is divided on the issue, that whether the above mentioned 2 cases, should be declared as a cure or long-term remission. Having only 2 cases as examples of fulfilling the above-mentioned criteria, it is a bit difficult to make out the difference.
The scientists themselves also agree that this strategy cannot be used in large scale for achieving a cure, even in the near future. The procedure of stem cell transplant carries very high risks and can’t be advised in every patient. Besides, stem cells having specific CCR5 mutations, which were used in the above-mentioned cases are very rare.
Scientists believe that, although bone marrow transplant can’t be given to all cases suffering from HIV, the results of the above cases has prompted researchers to look more deeply into CCR5 gene editing techniques, to modify immune cells to resist HIV infection. However, gene therapy contemplatedis not very easy to reproduce. The desired changes would have to be precisely directed at the cells in the right place (only the genes responsible for the production of CCR5 in bone marrow) and not other organs.

The medications used for HIV infection are much safer alternatives, as far as the mass application is concerned. Both the Berlin and London patient had undergone bone marrow transplant as a last resort, as they were critically ill with cancer& the transplant was for treating cancer in the patient and not the underlying HIV virus.
The scientists say, that a lot many questions are still unanswered and it may be premature to promise a cure to all people suffering from HIV infection. Even if by some method, the above-described procedure, can be successfully applied, one major flaw would still remain. This method is useful for only those cases, where the HIV virus uses CCR5 to enter the body. Unfortunately, sometimes HIV enters the body by using another different protein – CXCR4, for which the above method will not give satisfactory results. These people would still be susceptible to this kind of HIV called X4.
The observations described above have given hope to the scientific community that a cure for the most dreaded disease in the world – AIDS, is near. Many other HIV infected patients, who have received bone marrow transplant are being closely monitored by researchers. Foremost among them is – “Dusseldorf patient”who is now believed to be the 3rd person to be cured of HIV infection, following a bone marrow transplant; receiving cells from a donor with mutation of CCR5 gene. Biopsies taken from the gut and lymph nodes show no signs of infection. However, it is only just 3 months, that the patient has stopped taking antiviral drugs and the remission is still in early stage, which mandates further observation.
Unfortunately, the techniques described above are not just expensive and technically challenging but are also fraught with chances of severe unforeseen complications. Eventually, more time & research would be needed before, the steps are suitably modified to find solutions, which can be universally applied. But for now, we can rest with the optimistic belief that the end of HIV infection & its dreaded complication – AIDS, is not very far away.